Author: Rositsa Tashkova, Master of Molecular Biology and Microbiology
In recent decades, the value of stem cells and in particular - in the fight against certain cancers has been assessed. Treatment of cancer through stem cell transplantation has gained great popularity and success. In this article, we will look at when such treatment is needed and when it is even possible to perform such treatment, for which types of cancer is appropriate, what exactly is a stem cell transplant, and how it works.
In the article you will read:
- What are stem cells
- When stem cell transplantation can be used to treat cancer
- How stem cell transplantation helps treat cancer
- What types of stem cell transplantation are there
- What are the risks of stem cell transplantation
- What to expect during treatment
- What happens during the recovery period
- What happens if stem cell transplantation fails
What are stem cells
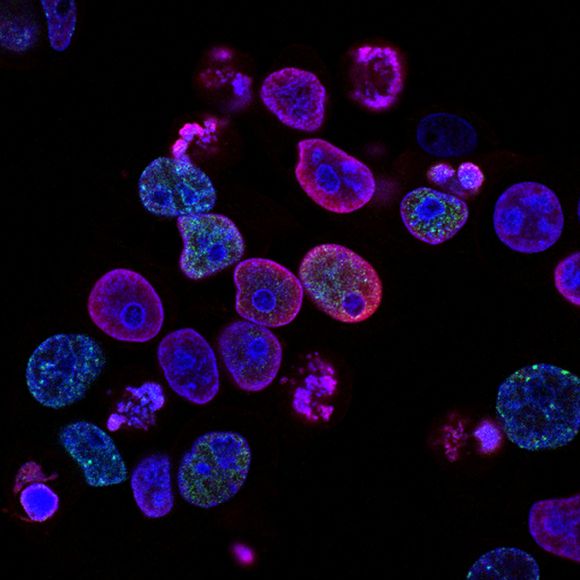
To understand how this treatment can help patients with certain cancers, we must first understand what stem cells are [ref. 1].
Stem cells do not specialize in performing a specific function, unlike, for example, red blood cells (erythrocytes), which carry oxygen to all parts of the body, or cells of the immune system that, in complex mechanisms, fight infections , or platelets, the only function of which is to participate in blood clotting, thereby protecting the body from major blood loss.
The process in which a stem cell develops in a strictly specialized cell similar to those described above is called differentiation. Thus, stem cells are undifferentiated, and erythrocytes are differentiated.
When stem cell transplantation can be used to treat cancer
Currently, stem cell transplantation is mainly used to treat blood cancer or one that affects the bone marrow - leukemia, lymphoma, multiple myeloma (also called multiple myeloma and Kaler's disease) or neuroblastoma (a disease that most often affects children).
Clinical trials are being carried out [ref. 2]in search of treatment and other cancers using stem cell transplantation, but no approved therapies have yet been established.

How stem cell transplantation helps treat cancer
Immediately before performing the transplant itself, the patient receives high doses of chemotherapy or radiotherapy for about a week. The goal is to destroy all cancer cells, including stem cells in the bone marrow, where blood cells are formed.
Previously, healthy stem cells were taken from the patient or from a donor to be transplanted immediately after chemo or radiotherapy. This occurs by instilling stem cells back into the bloodstream - intravenously.
After a while, they reach the bone marrow, where they occupy the place of the destroyed cells. There they begin to produce healthy blood cells, and with a successful transplant the patient is cured of cancer.
When stem cells are taken from a donor ( allogeneic transplant [ref. 3]) - usually brother, sister, parent, and are used to treat multiple myeloma or certain types of leukemia, an additional therapeutic effectcalled "graft vs. tumor" (GvT) may occur. With this effect, the white blood cells obtained in the transplant from the donor attack and destroy the rest after chemo- and radiotherapy cancer cells.
What types of stem cell transplantation are there
Stem cell transplantation is three types [ref. 4], depending on the source of the cells:
- Autologous transplantation [ref. 5] - when the stem cells are taken from the blood of the patient himself, before chemo- or radiotherapy. In this case, there is no risk of rejection of the transplant, since these are the own cells of the treatee.
- Allogeneic transplantation - when stem cells from a donor are used for transplantation. The donor must have similar molecules on his cells to those of the patient in order to reduce the risk of rejection. Therefore, most often a donor becomes the patient's brother, sister or parent, but a non-related donor from a registry whose cells must be compatible with the patient's organism can also be used.
- Syngenta transplantation - in rare cases, when the patient has a healthy single-day twin, stem cells are taken from it.

What are the risks of stem cell transplantation
Like any treatment, stem cell transplantation for cancer treatment hides its risks and has side effects [ref. 6].
Due to large doses of chemo- or radiotherapy that kill the patient's cells, problems with blood clotting and the immune system occur. This is because a large proportion of platelets and leukocytes have died. There is a risk of bleeding and infections.
Contrary to the effect "graft against tumor", another effect may occur, which is highly undesirable - "graft vs. host" [ref. 7] (GvHD).
This immune reaction can affect and damage many tissues and organs in the body - skin, liver, small intestine and others. In this case, it is necessary to take medications that suppress the immune system - immunosuppressants, which makes the patient susceptible to infections.
This effect can manifest itself a few weeks after transplantation or much later. Therefore, it is important that the stem cells that will be transplanted to the patient are as close as possible to his own.
All risks should be discussed in advance with the attending physician.
What to expect during treatment
Stem cell transplantation is a complex treatment and it should be taken into account that its cost can be very high. At the moment a modern stem marrow transplant is being performed in Varna, in the stem cell transplant center atSt. Marina Hospital [ref. 8].
Once an appropriate medical facility has been opened, the patient may be accommodated in the hospital or not, but frequent visits may be required. The whole treatment takes several months.
Before starting the course of chemo- or radiotherapy, it is necessary to secure the stem cells for the transplant. They are extracted from blood, bone marrow or umbilical cord and frozen. They thaw again before the transplant itself.
Chemo- or radiotherapy (can be administered and a combination between the two) take about 1-2 weeks, after which the patient rests a few days before transplantation.
The transplant itself takes between 1 and 5 hours, during which, with the help of a catheter, stem cells flow through a vein into the bloodstream - similar to an infusion of blood. Sometimes two insations are made at a certain interval of time.

The longest recovery process [ref. 10]. Its first phase is associated with the formation of new blood cells from the transplanted stemcells.
Since each organism reacts differently to transplantation, doctors can not predict exactly how the patient will feel as a result of treatment. It depends on many factors. For example, what state of health he was in before the transplant, how advanced the stage of cancer is, what type of cancer it is, what doses of chemo and radiotherapy had to be imied the patient, how they are perceived by the particular organism and other factors.
What happens during the recovery period
During the recovery period, the patient will remain for a long time under the supervision of doctors, who will monitor how his blood indicators change in time after the stem cell transplant. For the first three weeks, the number of blood cells will need to be counted every day or at least once a week.
Until the indicators return to normal, it should be vigorously guarded from infections and will feel weak and dropped. Negative and positive emotions can be intertwined in it - because of the relative isolation and physical malaise, but also in the hope of a successful outcome of the transplant.
In the first three months [ref. 11] blood or platelet insations may be required.
After a year or two, it is necessary to give the vaccines, which are usually put into childhood, because as a result of treatment with immune cells, immunity to pathogens acquired with these vaccines has gone before.
What happens if stem cell transplantation fails
Transplantation can fail for two reasons [ref. 12] - if our body rejects donor transplants or if the cancer returns.
In the event that our immune system recognizes foreign cells as hostile and attacks them, a new transplant or infusion of special white blood cells (lymphocytes) from the same donor can be undertaken.
Sometimes, years after the transplant, the cancer can return. In some aggressive cancers, when using the patient's own stem cells, relapse is observed in up to 50% of patients.
The most common cause of relapse remained in the body or in the transplant cancer cells. In this case, the effect "graft against tumor" is relied upon, in which the donor immune cells recognize and kill cancer cells. This effect can be strengthened if, together with stem cells, immune cells from the donor are also infused during transplantation.
In case of relapse, the condition can be treated by different chemotherapy, from the first time used, by a second transplant or both. If a re-transplant is selected and the first time the patient's own cells are used, then in this second transplant, donors can be used.